Understanding Embodied Pain
Trauma, Pain and the Mind-Body Experience
The phrase “mind-body connection” can feel ambiguous, but emerging science is now showing physiological connections between many seemingly unrelated mental and bodily issues—pain included.
As a group, there is a common and consistent finding that people with chronic pain tend to report much higher rates of past trauma when compared to people without chronic pain. Research also supports the connection between past trauma and an increased likelihood of transition from acute injury or illness to chronic pain.
This blog starts to explain the link between trauma and chronic pain. It’s a huge topic so understanding the neuro-science, addressing factors that shape pain and how they can be reshaped is good starting point. The role of occupational therapy is also briefly discussed as a key emerging therapy for people with pain and a history of recent or past trauma.
What is the overlap of Chronic Pain and Trauma
The following statistics show a high rate of trauma in people with chronic pain presentations.
90% of women with fibromyalgia syndrome report past trauma (1)
60% of those with arthritis report past trauma (1)
76% of patients with chronic low back pain report having at least one trauma in their past (2)
66% of women with chronic headaches report a past history of physical or sexual abuse (3)
58% of men/women with migraines report histories of childhood physical abuse, sexual abuse or neglect. (4)
56% of women who have chronic pelvic pain report sexual abuse in their past.(5)
This does not suggest that trauma directly causes chronic pain. However, it does suggest that a history of trauma might have some relationship to the development of chronic pain.
Understanding chronic pain, super briefly
“Pain, is a complex multi-dimensional experience, it is not the sole creation of our anatomy and physiology. It emerges only at the intersection of bodies, minds and cultures.”
~Morris, 1991.
Pain involves physical sensations, emotional responses to the sensations and social effects of the experience.
Melzack and Casey’s (2001) three dimension model of pain serves as a reminder of the complexity of pain. In this model we see that pain has a 3 main inputs:
-
Sensory input which relates to intensity, location, quality and duration of stimuli
-
Cognitive input which helps us evaluate the pain message and involves appraisal, cultural values, past experience, personality variables, context and cognitive state.
-
Affective input which relates to our stress response, involving the HPA axis, noradrenalin-sympathetic system, psycho-neuro-immune (PNI) system, cytokines, endogenous opiates and the limbic system.
These 3 dimensions are input to the “body-self neuro-matrix” and result in:
-
Pain perception
-
Behaviour – how we respond to the pain and what action we take to cope with the pain
-
Stress-regulation – involving levels of cortisol, noradrenaline, cytokines, endorphins and immune system activity
What is incredible is that these input and output dimensions all contribute to ONE single pain presentation.
The ”body-self neuro-matrix” is a complex adaptive system, which help us adapt to the many potential painful stimuli we experience on a daily basis. But if variants within this system do not support adaptation, pain can persist and become chronic. Pain is considered chronic when it persists for 3 months or longer.
Why does pain persist?
Persistent or chronic pain can be a result of complex neural networks involving changes in brain structure and function. Changes in nervous system keep nerves firing and signalling pain and can result in a phenomena called central sensitisation.
Central sensitisation (which is a key link to trauma) is a condition associated with chronic pain where the nervous system becomes stuck in a state of heightened reactivity. The sensations of pain can become more intense and things that are not normally painful, like touch, can also become painful
Central sensitisation is the mechanism which maintains pain even after the initial injury or illness heals.
It is now recognised that the brain “creates or perceives” pain via this sensitisation process and is determined by several factors, including;
-
Sensory elements: ‘danger signals’ from nerves, joints, muscles, and tissues.
-
Beliefs and cognition: past experiences with pain, context and anxiety
-
Emotions: both positive and negative feelings
-
Lifestyle: sleeping patterns, spirituality, stress levels, diet, exercise
-
Behaviour: doing too much or too little
The good news is that all these things that shape pain, can be reshaped. And that is what we do at Next Wave Therapy.
Here’s a 5 min you tube clip to understand this better
What is trauma?
Trauma is a state of high arousal in which normal coping mechanisms are overwhelmed in response to the perception of threat.
~ Cozalino, 2002:270
In a normal stress response to a perceived threat the amygdala activates the HPA axis – and results in a cascade of hormones which mobilise the fight/ flight reaction. This is designed to put us into action to keep us safe. It is an innate alarm response and when we are safe is inhibited by cortisol.
If however, the threat or danger cannot be escaped a freeze/ flop response occurs. In trauma this mobilisation to stress/danger persists, and cortisol does not halt the stress response. Many people who have suffered trauma feel guilt and shame for freezing or “going dead” and not doing more to protect themselves or others. Understanding this is a way of beginning the difficult process of self-forgiveness.
Most common types of trauma linked with chronic pain are early life stress e.g. abuse, neglect or parental loss; and life threatening events e.g. motor vehicle accidents, surgery, diagnosis of life threatening illness and physical illness.
What is relationship between Chronic Pain and Trauma?
We currently understand pain to be a result of complex neural networks involving changes in brain structure and function. Research shows that stressful life event set up a dysregulation in the stress response which contributes to these neural changes.
So if we consider pain as a dysregulation, as a failed response to stress and the symptoms of pain (as the body remembering) we can begin to see things differently
“In chronic pain, what we call the ‘body’ plays a mean trick on what we call the ‘mind.’ It tells the patient that pain is all in the body, when in fact over time pain is less in the ‘body’ and more in the mind. But always it is both.”
~ Dorene O’Hara
Nervous System as a Safety Officer
Nervous system is a risk assessor, continuously evaluating risk in the environment with the aim if keeping us safe, happy and well. Through nociception (neural surveillance mechanism), our brain identifies features of risk or safety (Porges, 2004). These is not learned but hardwired into our nervous system and reflect adaptive strategies associated with our phylogenetic history.
Polyvagal theory (founded by Porges) purports that the autonomic nervous system regulates 3 basic physiological states. Neuroception is the term he coined to describe how we use our body and brain to detect if situations are safe, dangerous, or life threatening and how to act in these situations.
We respond to each situation in the following ways:
-
Social engagement – which helps us to connect and seek help from others for safety.
-
Mobilisation – our stress (fight or flight) response which keeps us out of danger or harm.
-
Immobilisation – is activated in response to a life threat and involves freeze or faint defense mechanisms.
Early life stress, past histories of threat, and sometimes individual physiology, can leave individuals with systems of threat that work against them – that is, they are always aroused, on guard and ready to fight or flee.
Pulling it all together
Chronic pain is a real lived experience which has the potential to impact physical, mental, emotional and spiritual domains of a persons life. A past experience of trauma or early life stress can contribute to pain persisting due to the common denominator of the nervous system and the mind-body experience.
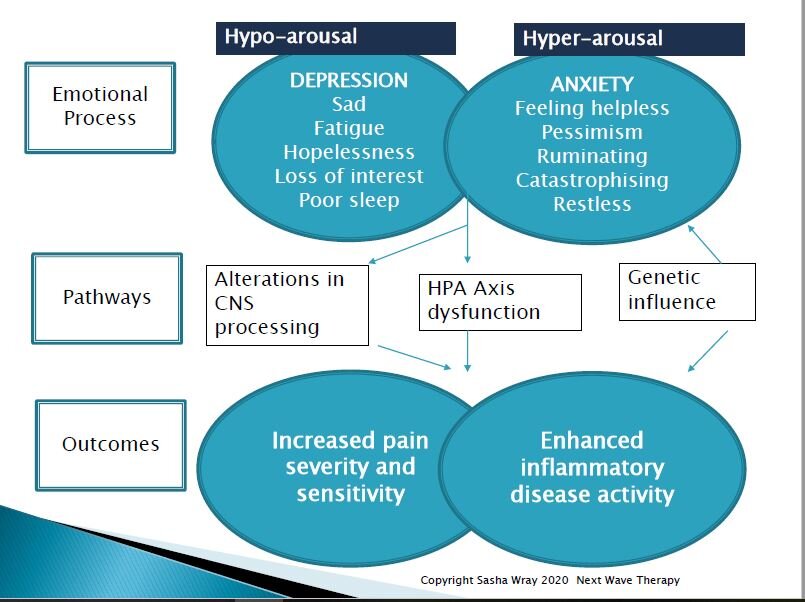
Trauma can lead to depression and/or anxiety with subsequent physiological arousal and changes in central nervous system processing, hypothalamus-pituitary-adrenal (HPA) axis dysfunction and epigenetics. Research has found that people with past trauma or early life stress have increased pain severity and sensitivity and enhanced inflammatory disease activity.
As such, when patients with a history of trauma get injured or become ill, their nervous system already in a state of persistent reactivity, is geared for pain and inflammation.
The diagram below illustrates the interplay of nervous system arousal, emotional states, body pathways and persistent pain outcomes.
Building vagal tone for pain management
The nervous system responds to our life experiences.
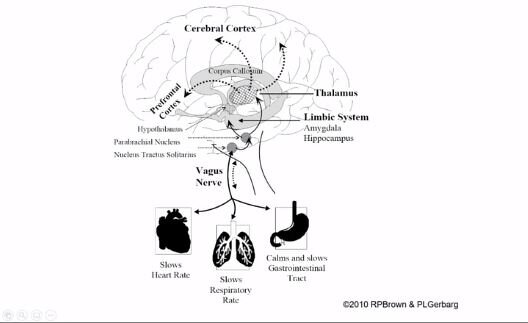
As we grow we learn to put the brake on our sympathetic stress responses. Responding to stress, danger or life threat is supported by a distinct neural anatomical pathways of the vagal system.
80% of the fibers of the vagus nerve are from the body to the brain and this helps us to train our arousal system.
~van der Kolk
Building “vagal tone” helps to regulate stress response, modulate emotions and adapt to life challenges. This can be done via the organs of the vagas nerve. These are the
-
lungs with breath, especially calm slow breathing to slow heart rate.
-
throat by talking with others, singing and voicing (naming what is happening in the body)
-
middle ear through listening, especially to calm voices and music.
-
face muscles through social engagement, smiling and spending time with people who make you feel safe and happy.
-
whole body through mind-body-breath activity such as exercises, yoga, dance, rhythmic movement and mindfulness of everyday activities.
Vagas 10th Cranial nerve “wanders” through the body to the brain.
Occupational Therapy and Mind-Body Experience
Occupational therapy as a profession grew in popularity from it’s whole person approach following World War II. Earlier, the power of occupation was recognised and used extensively in mental asylum’s. Fast forward 80 odd years and neuro-science is further validating this approach as valuable for trauma and pain management. That is, the therapeutic gains of the mind-body experience in everyday living.
At Next wave Therapy our occupational therapists focus on helping you to live your life fully, in whatever way you value. We offer many mind-body therapy such as yoga, relaxation training, acupressure, mindfulness, meditation and acceptance and commitment therapy. We use these with a trauma informed lens and always with the aim of empowerment or creating person centered change.
Most importantly these therapies help a person to feel not just in the physical body but to the presence of life within. When you participate in meaningful occupations – the small and the big – slowly over time you change the way you ‘are’ with those things and as a result the those things sustain and enliven you.
Copyright © Next Wave Therapy
Written by Sasha Wray
Sasha Wray is a director and principal occupational therapist at Next wave Therapy. Also a qualified naturopath and acupressure practitioner, Sasha has a special interest in helping people to live well. She treats complex pain presentations, chronic pain, mental health, trauma, neuro-endocrine and hormonal health concerns.
References
1. Walker, E. A., Keegan, D., Gardner, G., Sullivan, M., Bernstein, D., & Katon, W. J. (1997). Psychosocial factors in fibromyalgia compared with rheumatoid arthritis: II Sexual, physical, and emotional abuse and neglect. Psychosomatic Medicine, 59, 572-577.
2. Schofferman, J., Anderson, D., Hines, R., Smith, G., & Keane, G. (1993). Childhood psychological trauma and chronic refractory low-back pain. The Clinical Journal of Pain, 9, 260-265.
3. Domino, J. V., & Haber, J. D. (1987). Prior physical and sexual abuse in women with chronic headache: Clinical correlates. The Journal of Head and Face Pain, 27, 310-314.
4. Tietjen, G. E., Brandes, J. L., Peterlin, B. L., et al. (2010). Childhood maltreatment and migraine (part I). Prevalence and adult revictimization: A multicenter headache clinic survey. Headache, 50, 20-31.
5. Walling, M. K., Reiter, R. C., O’Hara, M. W., Milburn, A. K., Lilly, G., & Vincent, S. D. (1994). Abuse history and chronic pain in women: I. Prevalences of sexual abuse and physical abuse. Obstetrics & Gynecology, 84, 193-199.