Understanding Pain
Pain is a funny thing and an interesting topic of conversation in the clinic with patients.
When I tell patients that I experience pain on a daily basis, they seem horrified!
Maybe because as a physiotherapist they expect me to know the in’s and out’s of pain and therefore be able to avoid it or out smart it with some special “jiggery pokery” that I learned at physio school.
But pain is a good thing, it protects us, tells us to move or change our behaviour. It’s when it doesn’t serve this purpose that it starts to become a…………well………. bit of a pain!
Pain is normal
Without a doubt, pain is the primary reason people come to see us in the clinic. It’s not the only reason but it would definitely be number one on the list.
But what would you think if I told you that most pain is completely normal?
What if I told you that without pain the chance of survival of the human species would be severely reduced?
What if I told you that there is more to pain than just injured or “damaged” body parts?
Some of you might think that those previous statements are a bit left field but read on and I will give you a brief whirlwind tour of contemporary pain science.
Current Pain Science
The Internationally Association of the Study of Pain (IASP) have come up with the following definition of pain. This is not a final definition and is constantly under review as our understanding about pain changes.
“An unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage.”
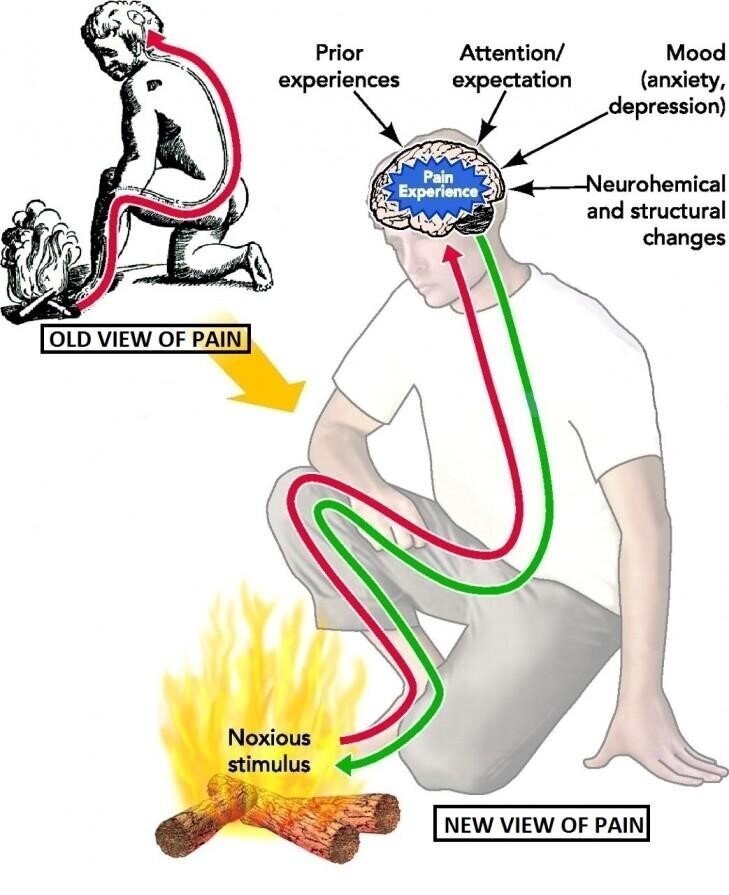
Commonly people understand pain to be a sensation from damaged or injured tissue caused by an external stimulus such as cutting your finger or stubbing your toe. Whilst this is often the trigger for a pain experience the actual process is not so straight forward.
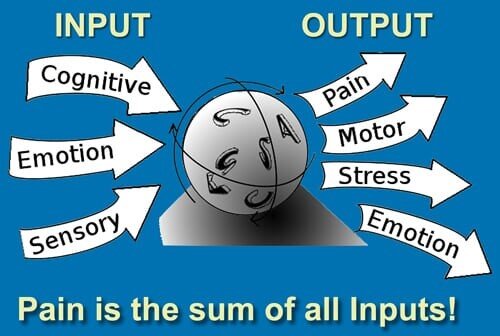
It would be more accurate to say that pain is not an input from outside the body but is an output from the brain based on multiple brain areas processing, analysing and evaluating the information that is entering the nervous system.
The IASP expand on their definition by saying
-
Pain is always a personal experience that is influenced to varying degrees by biological, psychological, and social factors.
-
Pain and nociception are different phenomena. Pain cannot be inferred solely from activity in sensory neurons.
-
Through their life experiences, individuals learn the concept of pain.
-
A person’s report of an experience as pain should be respected.
-
Although pain usually serves an adaptive role, it may have adverse effects on function and social and psychological well-being.
-
Verbal description is only one of several behaviours to express pain; inability to communicate does not negate the possibility that a human or a nonhuman animal experiences pain.
Old and new views of the pain experience.
The following description of pain is also quite interesting.
“Pain is a variable, conscious product of a stress response whose major purpose is to change the individuals behaviour…..when conditions allow….to the advantage and well-being of the tissues that are about to be damaged, are damaged, are healing, and / or are diseased or weakened in some way. The advantage of this to the whole organism’s survival is self-evident”.
Louis Gifford
Part of the above statement, “when conditions allow”, hints that it is not always convenient to have pain. For instance, moving out of a potentially dangerous situation may be perceived by your brain as being more important and therefore you may not experience pain until it is safe to do so. This also explains why people often don’t experience pain when they are distracted or pre-occupied by something such as a meaningful activity or when just passing time. The irony of this is that we see many people at Next Wave Therapy who have withdrawn completely from meaningful activities with the intention of resuming them when only when they have become “free of pain”.
Not all pain is the same
There are 4 main types of pain. These are nociceptive, inflammatory, neuropathic and nociplastic. I will briefly outline each one and the role that they play in the pain experience.
Nociceptive pain
The body has an early warning system that announces the presence of a potentially damaging stimulus. As well as sensory receptors important for touch and your awareness of your body in space, the body also contains high threshold receptors that respond to strong heat, cold, mechanical and chemical stimuli. These are called nociceptors and they are there to provide information to your brain on potentially dangerous stimuli.
Inflammatory pain
Your body is incredible at protecting you. If tissue damage results despite the nociceptive early warning system, then your body with shift its focus from protecting against potentially damaging stimuli to promoting the healing of injured tissue.
An Inflammatory process is used to accomplish this goal. Information passed along nociceptor nerves will produce reciprocal messages from the Central Nervous System back out to the periphery to facilitate this inflammatory response. Along with this, chemicals from cells of damaged tissue also trigger other specialized inflammatory cells to migrate to the site of injury.
This process results in increased sensitivity to the injured tissue so that stimuli that would not normally cause a pain experience, now will do so. The result of this is that the injured tissue is protected from further damage and allow healing and repair to occur. Inflammatory pain usually reduces as tissue healing resolves.
Neuropathic pain
Neuropathic pain is defined as, ‘pain arising as a direct consequence of a lesion or disease affecting the somatosensory system’.
Neuropathic pain can be both peripheral i.e. located in a nerve tissue outside of the spinal cord or central i.e. located in the brain or spinal cord.
Lesion is a term used that identifies evidence of an abnormality of the nervous system either through imaging, laboratory tests, biopsies, or where there is evidence of post traumatic injury or post-surgical injury to the nervous system. This injury to the nervous system causes changes that affect the way the nerve behaves and processes information. Pain can arise for no reason and is often described as shooting, burning, like electric shocks or ants crawling on the skin.
Nociplastic pain
Nociplastic pain is defined as ‘pain that arises from altered nociception despite no clear evidence of actual or threatened tissue damage to be causing the activation of peripheral nociceptors. There is also no evidence for disease or lesion of the somatosensory system causing the pain. This is suggestive of altered sensory processing i.e. the plastic changes have occurred in the nociceptive system.
No Brain No Pain
I’ve mentioned it a few times above and you’ve probably gathered by now that our understanding of pain is that it is not an input from the body tissues to the brain, which is a common misconception. Rather it is an interpretation of information coming from the body, which is then analysed and processed by multiple brain areas. If after this processing the brain interprets the information to be threatening to the body’s homeostatic status, then a painful response will be the output from this processing. Part of this brain process involves areas of the brain that analyse the context within which you find yourself i.e. what you see, hear smell and feel. It also involves memories of previous experiences, the beliefs that you have i.e. “bending my back is bad so if it hurts when I bend then something is getting damaged”.
All of this happens at a subconscious level and cannot be consciously “out thought”. The brain produces pain by activating a circuitry: a number of brain regions that become active all together when a person is in pain. These brain regions differ between individuals and possibly even for one individual in different circumstances, but they differ the most when comparing acute versus chronic pain.
We know that pain is a really poor indicator of tissue damage i.e. you can have a big injury and little pain or a small injury and a lot of pain. For some people pain continues beyond normal tissue healing times.
So, what has happened here?
Well, in acute musculoskeletal pain, the main focus for treatment is to reduce the nociceptive trigger. This focus on peripheral nociceptive pain generators is often effective for treatment of acute and sub-acute musculoskeletal pain. However, for patients that have persistent ongoing musculoskeletal pain, nociception i.e. potential or actual tissue damage, rarely dominates the clinical picture.
Chronic pain conditions are often characterised by brain plasticity that leads to hyperexcitability of the central nervous system. This means that stimuli that would not normally cause a pain experience may now produce a pain output.
Pain Management at Next Wave Therapy
Figuring out what is contributing to a pain experience is key to management. As mentioned above, acute pain that has only been present for a few days will be managed differently to pain that has been ongoing for months or years.
At Next Wave Therapy our Physiotherapists and Occupational therapists are highly skilled in the assessment and management of pain conditions. We work with you to help you address and manage factors feeding into your pain experience so that you can get back to doing what is meaningful and rewarding for you in your life.
Written by Jonathan Wray
Jonathan Wray is a director and principal physiotherapist at Next Wave Therapy. He is an APA titled Musculoskeletal Physiotherapist with a master’s degree in Clinical Physiotherapy. Jonathan has also completed specialisation training with the Australian College of Physiotherapists and is currently waiting to sit his final exams.
© Copyright Next Wave Therapy